Contact Us

Evidence that use of PIG improves early identification of patients in different settings and conditions in the UK and other countries.
|
Key findings – Use of the GSF PIG tool in different settings and with patients with different “Screening utilising the Gold Standards Framework PIG guidance in the |
There is good evidence that use of the GSF PIG (Proactive identification guidance or previously Prognostic Indicator Guidance) improves early recognition or identification of patients considered to be in their last year of life. However, this is only the first key step in the GSF Quality Improvement Programme used in different settings (primary care, care homes, hospitals, domiciliary care, prisons hospices etc.). Intrinsic comparative evaluations of teams progressing with the GSF programme demonstrates significant change towards current population-based estimates (e.g., 1%, 30%, 80%), and that high levels of early identification in line with this can be achieved. The further steps of GSF, including use of Needs-support matrix, MDT discussions, ongoing assessment and proactive planning, all then work together to ensure better care for patients in line with their preferences.
1. Evidence from peer-reviewed published literature that use of the GSF PIG (Proactive identification guidance) supports earlier identification of patients considered to be in their last year of life.
|
Date |
Location – |
Study group |
Finding / Conclusion/ Message |
Reference |
|---|---|---|---|---|
|
2015 |
Hospital Australia |
Geelong Australia -study in a general hospital admissions |
The use of an objective clinical tool identifies a high prevalence of patients with palliative care needs in the acute tertiary Australian hospital setting, with a high 1 year mortality and poor return to independence in this population. The low rate of documentation of discussions about treatment limitations in this population suggests palliative care needs are not recognised and discussed in the majority of patients. |
Sharyn Milnes et al A prospective observational study of prevalence and outcomes of patients with Gold Standard Framework criteria in a tertiary regional Australian Hospital |
|
2012 |
Hospital UK |
|
A modified GSF PIG identified most patients in last year pf life |
Mason C Shah S |
|
2012 |
Hospital UK |
Acute Coronary Syndrome |
This study has highlighted a potentially large number of ACS patients eligible for EoL care. GSF or GRACE could be used in the hospital setting to help identify these patients. GSF identifies ACS patients with more comorbidity and at increased risk of hospital readmission GSF PIG effective in identifying pts with ACS EOL |
Fenning S, Woolcock R, Haga K, Iqbal J, Fox KA, Murray SA, Identifying acute coronary syndrome patients approaching end-of-life. PLoS One. 2012;7(4):e35536. doi: 10.1371/journal.pone.0035536. Epub 2012 Apr 18. |
|
2012 |
Hospital UK |
Emergency admissions |
Qualitative study to explore the perspectives of patients palliative care needs were received while in hospital. |
Richards N., Gardiner C., Ingleton C., Gott M. Palliative Medicine, June 2012, vol./is.26/4(537- 538),0269-2163 |
|
2013 |
Hospitals UK |
Hospitals - high symptom burden |
The paper highlights elevated levels of burden experienced by patients with palliative care requirements. Moreover, the paper also indicates that a large proportion of such patients are not in receipt of palliative approaches to their care i.e., GSF PIG helps identify patients with a high symptom burden in hospital. |
Ryan T., et al Symptom burden, palliative care need and predictors of physical and psychological discomfort in two UK hospitals. |
|
2013 |
New Zealand |
Acute hospital |
One fifth of hospital inpatients met criteria for palliative care need, the majority of whom were aged >70 years. |
Gott M et al BMC Palliat Care. 2013 Mar 28;12:15. doi: 10.1186/1472-684X-12-15.Palliative care need and management in the acute hospital setting: a census of one New Zealand Hospital.
|
|
2012 |
Community UK |
Heart Failure |
Identifying community based chronic heart failure patients in the last year of life: a comparison of Gold Standards Framework Prognostic Indicator Guide and the Seattle Heart Failure Model. Predicting heart failure patients nearing end of life is difficult- GSF PIG can help (86% identified for final year ) but more help might be useful to improve identification. |
Heart. 2012 Apr;98(7):579-83. doi: 10.1136/heartjnl-2011-301021. Haga K1, Murray S, Reid J, Ness A, O'Donnell M, Yellowlees D, Denvir MA.
|
|
2013 |
Hospitals UK |
Acute Hospital |
GSF helps identify a third of all patients (NB Pre Clarke- paper) The results reveal that according to the GSF prognostic guide, over a third of hospital in-patients meet the criteria for palliative care need. |
Gardiner C et al Extent of palliative care need in the acute hospital setting: a survey of two acute hospitals in the UK. |
|
2014 |
New Zealand hospital |
Acute Hospital |
The sensitivity, specificity and predictive values of the Gold Standards Framework PIG guidance in this study are comparable to, or better than, results of studies identifying patients with a limited life expectancy in particular disease states (e.g. heart failure and renal failure). Screening utilising the Gold Standards Framework PIG guidance in the acute setting could be the first step towards implementing a more systematic way of addressing patient need - both current unrecognised and future anticipated - thereby improving outcomes for this population |
O'Callaghan A et al
|
|
2014 |
Hospital -Italy |
Acute Coronary Syndrome |
A study to find the most accurate method of identifying the last year of life in patients presenting with acute coronary syndrome: A multi-centre prospective study. |
Moretti |
|
2014 |
Hospital UK |
COPD |
This study showed wide variation in survival in a patient population on LTOT. The ADO score could be used as an early trigger for referral to palliative services, thus enhancing end-of-life care, which improves quality of life in COPD. A prospective study of this application would be required to prove this hypothesis Ie GSF PIG and other tools helps predict COPD patients in the last year of life |
Law S1, Boyd S, Macdonald J, Raeside D, Anderson D Predictors of survival in patients with chronic obstructive pulmonary disease receiving long-term oxygen therapy. BMJ Support Palliat Care. 2014 Mar 25. doi: 10.1136/bmjspcare-2012-000432.
|
|
2014 |
Hospital - New Zealand |
General admissions |
Can we predict which hospital patients are in their last year of life? A prospective cross-sectional study of the Gold Standards Framework Prognostic Indicator Guidance as a screening tool in the acute hospital setting |
O Callahan |
|
2015 |
Hospital UK |
Liver Disease |
Screening for poor prognosis can improve end of life care for patients with chronic liver disease. |
Hudson et al |
|
2016 |
Hospital -Italy |
(STORM) Acute Coronary Syndrome patients |
A study into risk assessment in acute coronary syndrome in patients towards the end of life. |
Moretti et al |
Note - The key paper by David Clark in 2014 confirms that 29% of all hospital patients are in their last year of life, and this provides us with the evidence on which to base our aspirations for early identification rates in all our GSF Hospital programmes. Ref Clark et al Imminence of death among hospital inpatients: Prevalent cohort study. Palliat.Med. 2014 Mar 17:28(6):474-479
2. Evidence from Intrinsic GSF Evaluation Audit
Early identification is GSF’s first key step. The GSF training and coaching enables staff to increase their identification rate over time, supported by use of the GSF Proactive identification guidance and abbreviated forms of it (e.g., Mini-PIG, PIGLET) through teaching, coaching, use of run-charts, workshop feedback, peer-support, etc. Over the course of a GSF Programme (6-24 months dependant on organisation and delivery), teams are able to demonstrate improvements in care at:-
- Patient level
- Organisational level
- Staff level
The data is captured before and after the delivery of the programme and at accreditation to demonstrate sustainability.
a) Acute Hospital wards - Cumulated data from 10 GSF Accredited Hospital wards.
The snapshot average 34% of all patients (in line with Clarke study 2014, confirming that 29% of patients in hospital are in their last year of life).
Fig 1. Identification rate in GSF Accredited acute hospitals for patients in the last year of life. 2015-17
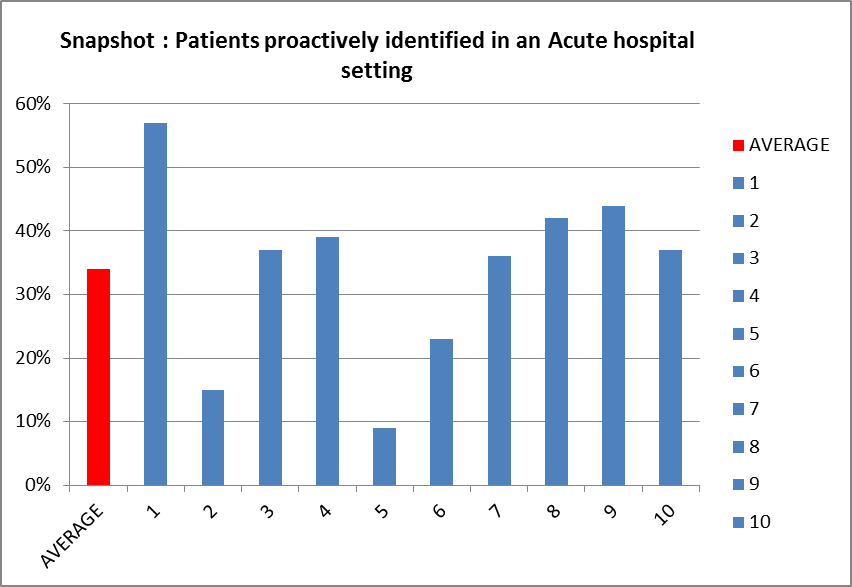
Fig 1. Demonstrates what is achievable on an acute hospital ward. The wards identified covered a range of specialities including oncology, haematology, stroke rehabilitation, renal unit, general medicine, orthopaedic and elderly care, AMU and a respiratory ward. The range of identification rates was between 9% and 57%, the average was 34%.
b) Community Hospital wards
Fig 2. Identification rates in GSF Accredited Community Hospitals 2015-16
.png)
Fig 2. Demonstrates what is achievable in community hospital wards. The wards are from the last two rounds of GSF accreditation.
The identification rates range on average from 31% to 100%. The weekly identification range across the 8 hospitals ranged from
23% to 100%.
c) Primary care
Cumulated data from 17 GSF Accredited GP Practices (more details available).
Conclusion for these GSF GP Practices – an average identification rate of 60% of all patients (in line with population figures of estimate 1% population dying/year)
Fig 3. Identification rates ion Primary Care in 17 GSF Accredited GP practices
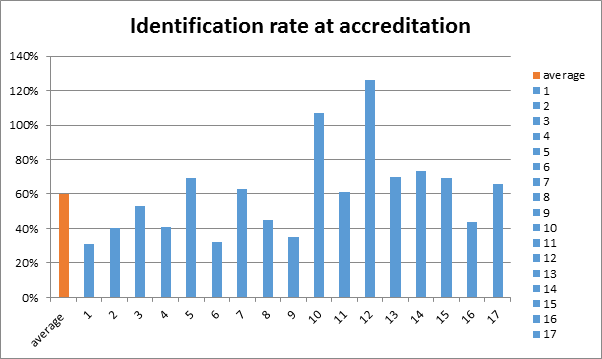
Fig 3. Demonstrates that some GP practices, following GSF Going for Gold training and Accreditation, are attaining high rates of identification of patients for their GSF/Palliative Care Register, averaging 60%. This demonstrates what is possible to achieve by some GP practices, which could be an encouragement to others.
Fig 4. Findings from GSF Reaccredited GP practices 2016
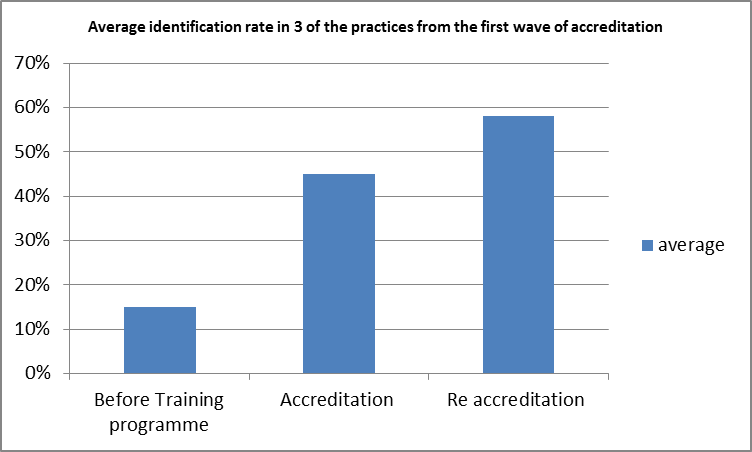
Fig 4. Demonstrates that GSF is sustainable with 3 of the original 7 practices have gone for re accreditation 3 years on.
For Care Homes consideration of early identification is different: all residents are considered to be approaching the end of their life and coded appropriately , with many considered to have years to live (blue code) and about 80% considered to be in their last year of life. The Needs Based Coding relates to the predicted stage of decline. An assessment at accreditation is made of the allocated coding for people when they die (red/amber) through the After Death Analysis and most care homes are found to estimate decline appropriately. See Summary of Evidence Care Homes for more details.
3. Evidence for conference abstracts, grey literature and qualitative research
|
Accredited GSF Hospitals Source: Ref Thomas Armstrong Wilson National GSF Centre in End of life care GSF Accreditation |
HW Wright, Palliative Care Team Leader, Barking Havering and Redbridge Hospitals - said following GSF accreditation of their first ward: “We believe that the GSF has developed within the hospital a greater awareness for the need to have conversations about death and dying in order to plan end of life care. By raising awareness this has enabled clinicians to gain confidence in identifying patients earlier in their disease trajectory and helped to prompt effective end of life communication where needed.”
LB Practice Nurse at Grosvenor Medical Centre
“When the practice started GSF there were only 13 patients on the register. There are now 51 and the proportion of non-cancer patients has risen from 25% to 53%.
The biggest benefit of doing GSF has been the continuity of care. Whereas in the past we would tend to hand over responsibility to the district nursing team, now a named GP and the nursing team at the practice is involved throughout and the patients feel much better cared for. Now the DNs enter our team not the other way round.”
HMP Norwich
Lead Nurse SR, said: “GSF has helped us do everything that little bit better. We are certainly better at identifying people approaching the end of life because we now look more closely and have a mental checklist. It’s also helped us to be better planned and more organised – things really flow now. It’s really helped the team feel justifiably confident in the care they are providing. Having their work acknowledged means they can boast about it.”
Airedale General Hospital
GSF helped increase identification of patients in last year of life to 30%. Dr RM, Consultant Geriatrician at Airedale, said: “The GSF and Gold Line provides me with the added reassurance that my patients and their family have a plan, and the added resources in place as they move from secondary care to the community.”
Saltaire Medical Practice.
Increased number of patients on the register from six to 84. Dr IL, said: “We only have one chance to get it right. With an ageing population, this is becoming an increasingly important part of our work as GPs and so we have to ensure consistency and equality
Ilkley Moor Medical Practice
Prior to doing the GSF Going for Gold programme, we had 27 patients on the GSF register, almost all of whom were cancer patients. Now we have 236 on the register, 70% of whom are non-cancer.


